What is your research about?
The area I’ve been studying for a while is women’s health, before and after pregnancy. It started with depression, and that has led to looking at other important pieces of women’s health. I’m looking at ways we can use psychology to help improve the experience of motherhood and health outcomes.
When did breastfeeding become more of your focus?
It started with just trying to learn more about postpartum depression and the things that go along with it. I’d been working with Riverside Methodist Hospital in Columbus for about five years. Our first project was looking at first-time parents and looking at all the psychological and social predictors of their well-being.
We were initially looking at depression, but we looked at breastfeeding as well, mostly because the hospital was interested in having some more information on the topic. From that, we realized how closely related mental health and breastfeeding outcomes are and how they’re related to the relationship between a mother and her partner, if she has one. We’ve found that one of the things that predicted if a new mom was still breastfeeding at six months was self-efficacy, or how confident a mom feels in her ability to breastfeed, and whether or not she experiences depression.
Where do breastfeeding rates currently stand?
Most moms try it. A lot of moms begin breastfeeding within the first couple of days postpartum. Most hospitals report about 80 percent of mothers in the U.S. start out breastfeeding, and similar rates were found at Riverside. Between six weeks and three months postpartum, that number goes down to maybe 60 percent. By six months postpartum, that number nationally goes down to around 18 percent. In this group, it was about 30 percent. In general, the most routinely recommended length of time for breastfeeding is at least six months for the baby’s and mom’s health. Women are finding that hard to do, in the United States especially.
How did all of this evolve into a web-based program?
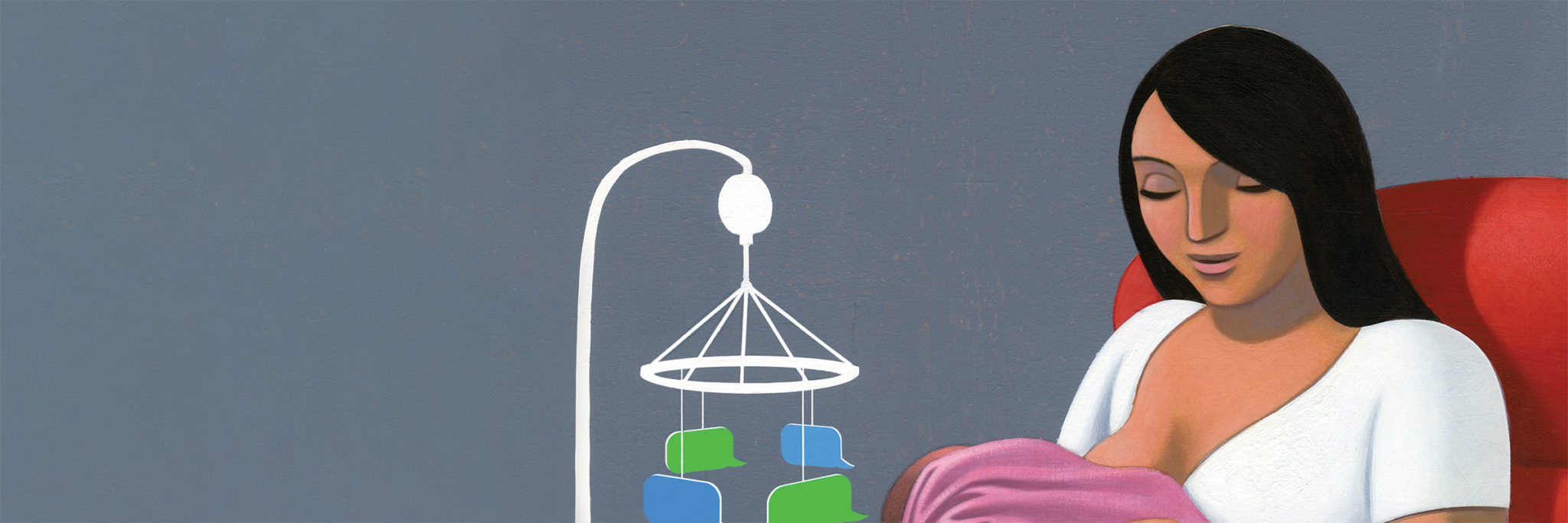
We started with surveys and followed up with interviews and focus groups of parents, learning from them what their first year of parenthood looks like. After that, we had a pretty good idea of what types of information would be helpful to parents and how they wanted it delivered. Parents wanted information in tiny, manageable bits rather than through a class or a weekly workshop they have to attend. We listened to what parents were saying about what’s hard, challenging, and awesome about parenthood, and we wanted to come up with something that might feel more manageable than what has traditionally been offered. We began to think we could tip the scales with something like an app or a mobile program.
How does it work?
Parents are given an iPad, two days after delivery, to complete a profile, answering questions about their breastfeeding concerns, the ways they best deal with stress, and how they each feel best supported by their partners. Parents receive four tailored text messages a week, populated by their initial profile, for the next three months to give them encouragement and support. It gives them reminders to use coping strategies they’ve used in the past, to help them reflect on their motivations for breastfeeding, and to give them tailored information about the challenges they mentioned.
For example, if a mom is having difficulty latching early on, she’ll probably get more messages in the first couple of weeks about how to know if her latch is working right, or she might receive a video on proper latch. Whereas, if a mom is more concerned about milk supply, we might remind her more frequently about the hospital’s baby weigh station or the normal amount of time between feedings. The messages are all based on what they’ve told us initially in the hospital.
The program gives moms milestones to reach for, such as breastfeeding at one month or two months. It gives them congratulations and confidence builders. But it also offers prompts for the mother’s partner or co-parent to listen supportively about things that are difficult about breastfeeding. It simply reminds the partner that, even if they are not the one actively breastfeeding, the partner can be supportive by offering to change the baby afterward, bringing a glass of water, or sitting with mom if she wants some company. These little things can give mom the sense that she’s not in this alone and that she’s doing something important.
The program also connects parents with existing hospital resources through links to information on baby weigh-ins, free phone or walk-in lactation support, and breastfeeding support groups. Sometimes when parents leave the hospital, they’re given a whole host of information, videos to watch, and paperwork to sign, so sometimes that information gets lost when they need it. We provide continual reminders, so if parents want to make use of those resources, they can. With small, little interventions, we can’t replace hands-on, one-on-one consultation, but we can supplement it to make even better use of those resources.
Is it up and running now?
It’s in process. Since this is research I’m passionate about, I’ve been bringing students into the project at every stage of its development. Several students were instrumental in designing a functional prototype of the web-based program. The students piloted all of the steps that would be involved in setting up a randomized, clinical trial, in which half of the people receive the new program and the other half receive care as usual, which are all the things the hospital normally does for breastfeeding moms. We followed the outcomes for three months the first time.
Now, Riverside has committed funding through the OhioHealth Foundation to the professional development of the program. A technology company will take our prototype and turn it into a fully functional program. The foundation is also going to fund the next phase of our clinical trial with 250 moms. That will let us know whether this produces better outcomes compared to care as usual. If that’s the case, then we will make it widely available. Breastfeeding is a learned skill. It’s not mind over matter. For moms who choose to do it, we hope we can tip the balance in their favor a little bit with something that costs them very little time and no money.